photo caption: As part of a team approach for selecting an AFO, the physical therapist contributes insights that include information about the gait cycle.
by Polly Swingle, PT, GCS, CEEAA
An ankle-foot orthosis (AFO) is a specialized support designed to provide corrective foot and ankle positioning and support for safety, stability, and efficiency of movement for those with compromised mobility—specifically individuals with musculoskeletal or neuromuscular dysfunction.
An AFO can be used to:
• Substitute for impaired muscle performance in the presence of weakness to improve foot clearance in the swing phase of gait.
• Provide stance phase stability and support to enhance alignment of limb segment when there is structural instability in one or more lower extremity joints.
• Limit joint motion or unload forces during weight bearing to allow healing after surgery or prevent injury to vulnerable joints.
• Enhance mobility by minimizing the impact of abnormal movement associated with hypertonicity by positioning limb segments for optimal function in persons with impaired motor control and abnormal tone.
• Minimize the risk of development of bony deformities and contracture associated with long-standing hypertonicity, especially in growing children.
There are many different reasons to use an AFO and a number of important factors to consider when selecting one for a patient. Physicians and therapy professionals should understand the differences between the different types of AFOs, design and selection factors, what that selection process looks like, and who should be involved in the consultation, evaluation, and selection process.
Types of AFOs
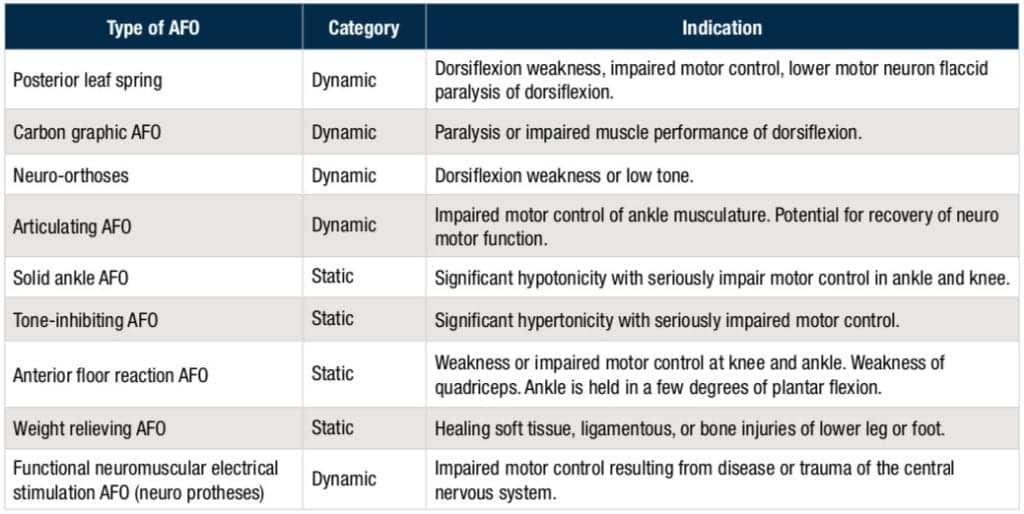
AFOs can be divided into two broad categories: static devices, which prohibit motion in any plane at the ankle (this category includes solid ankle AFOs, floor reaction AFOs, and patellar tendon-bearing AFOs), and dynamic AFOs. Dynamic devices like a posterior leaf splint or an articulating AFO allow some degree of sagittal plane movement in the ankle. The primary goal of a dynamic AFO is to provide enough external support in stance and clearance in swing with minimal compromise of forward progression through the heel, ankle and toe rocker of gait.
The following chart includes a selection of common AFO types, including a notation about whether the device is a static or dynamic AFO, and what medical/therapeutic indication the AFO is designed to address.
Material and Fit
Because the effectiveness of an AFO is largely determined by the intimacy and consistency of its fit, understanding the differences and trade-offs between a prefab orthotic and a custom-molded device is essential.
Prefab orthoses are available in a wide spectrum of orthotic designs, are correlated to shoe size, and are made of a number of different materials. Because the degree to which they can be modified or adjusted to fit an individual varies considerably, a prefab AFO may be problematic for persons with foot deformity, extremely wide or narrow feet, or large calf muscles. While clinicians generally do not prefer these AFOs due to concerns about a possible poor fit, they are available at a significantly lower price point, which can be attractive to patients with limited insurance coverage or financial limitations.
Custom-molded orthosis provide optimal control of the limb. Because of their intimate fit, these AFOs are especially important for patients with poor sensation, significant hypertonicity, or who are at risk of progressing deformities associated with their condition. The orthotist constructs the orthosis around a rectified mold of the patient’s limb, assuring adequate pressure relief over vulnerable areas. Thermoplastic AFO can be very effective in controlling a wide range of orthopedic deformities. However, because that efficacy requires a total-contact, intimate fit in all three planes of motion, intimacy or contact between limb and orthosis is best achieved with a custom-molded design. The only true contraindication of a custom-molded thermoplastic design is significantly fluctuating limb size associated with conditions that lead to edema of the braced extremity. When the limb size fluctuates, the intimacy of the custom-molded fit is lost.
Selecting the Right AFO
Given the wide range of different AFO types available, health care professionals should be thoughtful when identifying and recommending an AFO to a patient. There are a number of factors to consider, and a collaborative, team approach is strongly recommended to optimize the chances of picking the “right” AFO for an individual.
Doctors and therapists should first clearly define what they want an orthosis to accomplish, factor in important practical considerations like cost and comfort, and review the many available options to select the design and components that will best meet each patient’s needs, preferences and goals.
Generally speaking, selecting an AFO requires consideration of the following four factors:
• Potential advantages or positive outcomes expected when using the orthosis (how it might improve walking, correct posture, or protect a limb).
• Any disadvantages or trade-offs that may be associated with its use (expense, impose limitations or complications on daily activities, the energy cost of using the device).
• Indications that the orthosis may be useful to the patient, taking into account individual factors like medical, personal and financial circumstances.
• Any personal circumstances or unique individual characteristics that make use of the device detrimental or contraindicated.
Physical therapists have several sources they can turn to that provide AFOs that meet a range of patient needs. One source is Allard USA, Rockaway, NJ, which offers foot drop AFOs that provide products for mild, moderate, or maximum stability including AFOs made of carbon composite. Another manufacturer, Cascade Dafo Inc, Ferndale, Wash, also offers a line of ankle foot orthoses focused on the pediatric market.
The ideal AFO provides the right balance of:
• Functionality: the device meets the patient’s mobility needs and goals, maximizes stance phase stability, minimizes abnormal alignment, minimally compromises swing clearance, effectively prepositions the limb for initial contact, and is energy-efficient.
• Comfort: device can be worn for extended periods and is easy to put on and remove.
• Cost: device can be created and maintained with minimal cost.
• Cosmesis: device satisfies the individual’s need to fit in with his or her peers.
• Accessibility: Minimal fabrication demands. The device can be made in a short period of time using a minimally complex design, and provides some degree of adjustability to enhance initial fitting.
[sidebar float=”right” width=”250″]Product Resources
The following companies provide products to treat ankle injuries, drop foot, and other aspects of stroke and neurological rehabilitation:
Active Ankle
www.activeankle.com
Allard USA Inc
www.allardusa.com
GAITRite-CIR Systems Inc
www.gaitrite.com
Gorbel Rehabilitation/SafeGait
www.gorbelrehabilitation.com
Mobility Research
www.litegait.com
Motorika Medical Ltd
www.motorika.com
Ottobock
www.ottobockus.com
ProtoKinetics
www.protokinetics.com
Saebo Inc
www.saebo.com
Solo-Step
www.solostep.com
Tekscan
www.tekscan.com
The Medi-Kid Co Inc
www.medi-kid.com[/sidebar]
A Team Approach
When an individual with neuromuscular or musculoskeletal dysfunction has difficulty with walking or with overall mobility, decisions about their orthotic options are best made in a collaborative manner—with input from an interdisciplinary team. Ideally, that team would include the physician involved in his or her care, the physical and/or occupational therapist who is likely to be involved in functional training, the orthotist who will design, fabricate, deliver, and maintain the orthosis, and, last, but certainly not least, the person who will be using the orthosis, as well as their family members or caregivers.
The physician brings an understanding of the specific disease or disorder that the patient is dealing with, including the natural history and likely prognosis, the type of secondary musculoskeletal problems that are commonly encountered, and any cognitive, developmental, or multisystem involvement that may be associated with the disease.
A physical therapist contributes insights gleaned from patient examination to provide critical information about muscle performance, motor performance and control, range of motion, limb alignment, information about the gait cycle—with attention to both primary patient impairments and the compensation strategies the individual uses while walking—as well as how the orthosis might biomechanically impact other daily motor tasks.
As the one who is fabricating the device and has the best understanding of the materials and design specifics—including any potentially beneficial new products and materials—an orthotist is also a valuable member of the team.
The patient and family members or caregivers can provide important information about practical issues, such as who will be responsible for applying or removing the device and the ease with which this can be accomplished. Details about the patient’s lifestyle (from things like extreme levels of activity with sports and recreation, to the need to use stairs frequently, or even the need to change shoes more often than usual) can all make a big difference on the type of AFO best suited to meet his or her needs.
Costs, Considerations and Final Thoughts
The AFO selection process cannot be conducted in a vacuum. There is almost always some cost to patients, and financial considerations and capabilities cannot be ignored.
It’s also important to recognize that every patient and every situation is unique. Off-the-shelf options can be helpful in some circumstances, but medical and therapy professionals should proceed with caution. Physicians should be leery about definitive or prescriptive recommendations without first consulting a team as outlined above.
Lastly, the importance of comfort and patient education cannot be understated. The patient is the one who has to wear the device, and if it is prohibitively uncomfortable or inconvenient, many patients will not wear the device as prescribed. Patients should understand that minor modifications to the device can make a big difference in fit and comfort level and should feel comfortable going back to their therapist and/or orthotist to assist with those adjustments.
Whether by ensuring gait stability, keeping joints in proper alignment, helping to compensate for muscle weakness or imbalance, or correcting deformities, the right AFO can be extraordinarily beneficial for patients dealing with musculoskeletal or neuromuscular dysfunction. In addition to medical benefits, a thoughtfully selected AFO can improve comfort, mobility, and even quality of life—which makes understanding what goes into that selection process critically important for physicians and therapy professionals. PTP
Polly Swingle, PT, GCS, CEEAA, is co-founder and lead physical therapist of The Recovery Project (visit www.therecoveryproject.net), which provides progressive, effective, evidence-based neuro rehab therapies that improve the quality of life and functionality of patients with spinal cord, neurological and traumatic brain injuries at its three Michigan-based locations. For more information, contact [email protected].




