Facilitating gait and balance recovery post-stroke
Approximately 795,000 individuals suffer new or recurrent strokes each year in the United States. Gait and balance deficits are the main causes of decreased independence and quality of life, and increased risk for falls in patients with stroke.1 To facilitate motor recovery, physical therapists incorporate well-researched neuroscience principles of task specificity, complexity, and intensity to guide treatment interventions. The focus of this article is to provide an overview of the wide array of gait and balance technologies available in stroke rehabilitation.
Gait Technologies
Today’s gait training devices range from models designed with very low technology to the highly advanced, and incorporate concepts of task specificity and mass practice to facilitate recovery of walking and induce cortical reorganization following stroke. The physical therapy staff at Madonna Rehabilitation Hospital, Lincoln, Neb, utilize both manual body weight support and robotic assisted gait training devices.
The partial body weight support system available through Robomedica Inc, Mission Viejo, Calif, is a manual gait training device in which a patient is harnessed and supported over a treadmill, and provided a percentage of body weight support while ambulating. Up to three therapists are used to facilitate the hips and lower extremities through a normal gait pattern. The percentage of body weight support, treadmill speed, duration, and the amount of manual facilitation required from the therapists can be adjusted to challenge and progress the patient.
The LiteGait by Mobility Research, Tempe, Ariz, is another manual body weight support system. It can be used over ground or over a treadmill and incorporates a harness system to support the patient during gait.
The ZeroG, available through Ashburn, Va-based Aretech LLC, is a body weight support device used to facilitate gait training. It includes an overhead trolley and harness system that allows for both static and dynamic body weight support. Advanced technology is used to monitor the patient’s movement to assure a high level of patient safety and record patient-specific data to demonstrate progress toward recovery.
An additional technology that makes use of dynamic body weight support through an overhead rail, incorporating a harness and actuator, is the SafeGait 360° Balance and Mobility Trainer from Gorbel Medical, Fishers, NY, with patient-management software built to allow patient performance measures to be tracked and compared by task and session.
Sioux Falls, SD-based Solo-Step’s ceiling-mounted Solo-Step system also provides a performance harness for safety, a lanyard which connects the harness to the trolley, and a track comprised of heavy-duty aluminum.
The AlterG anti-gravity treadmill by AlterG, headquartered in Fremont, Calif, uses differential air pressure unweighting technology. The patient uses two steps to get onto the treadmill and is zipped into a bag that provides lower-body positive pressure support. The therapist is only able to provide verbal cueing and does not have access to the lower extremities to provide manual facilitation. The patient looks at a monitor during gait training that provides visual feedback of their lower extremities.
Manual body weight systems are appropriate for stroke patients with hemiparesis, ataxia, motor control deficits, lower-extremity weakness, deconditioning, and/or sensory and proprioceptive deficits, and are most appropriate for patients with minimal deficits. They can be extremely labor intensive, resulting in overuse injuries for the clinicians. According to Judith M. Burnfield, PT, PhD, et al, repetitively lifting a patient’s leg through awkward postures even at relatively slow speeds is fatiguing for clinicians and has led to injury. In addition, with up to three therapists required for this type of training, it may not be optimum technology for facilities where cost containment and productivity are emphasized.2
Due to the risk of overuse injury with manual body weight support systems, the use of more advanced technologies is an important consideration. The Intelligently Controlled Assistive Rehabilitation Elliptical (ICARE) by SportsArt Fitness was developed at Madonna Rehabilitation Hospital Institute for Rehabilitation Science and Engineering.
Watch the ICARE in action.
The ICARE is a motorized elliptical trainer that simulates a kinematic movement pattern similar to normal gait. It has several specialized features, including an intelligently controlled motor, body weight support system, adjustable stride length, adjustable seat, adjustable pedal straps, options for upper-extremity positioning, a ramp for easy access, and a platform in front for the clinician to communicate with the patient.
Lokomat by Hocoma Inc, Norwell, Mass, is a robotic gait trainer with externally powered orthoses to guide each leg in a gait-like movement pattern while the patient walks on a treadmill with a portion of their body weight supported. The AutoAmbulator by HealthSouth, Birmingham, Ala, is another available robotic gait training device on the market that functions similarly to the Lokomat. These devices would be appropriate for stroke patients who are low functioning with little trunk control, significant lower-extremity weakness, ataxia, decreased balance, and/or impaired motor control. Both technologies allow patients to be upright and walking early in their recovery, and help decrease the deleterious effects of inactivity and immobility.
The Ekso, manufactured by Richmond, Calif-headquartered Ekso Bionics, is a wearable exoskeleton that assists the patient with standing and walking. Walking is achieved by the patient shifting weight, which activates the sensors to initiate a stepping pattern. The patient must have good cognitive ability to respond to verbal and auditory feedback. This is the main difference in indications for use compared to the Lokomat and AutoAmbulator. The benefit of the robotic-assisted devices—the Lokomat, the AutoAmbulator, and the Ekso—is the reduced physical demands on the clinician, yet they can be costly.
Balance Technologies

The Proprio Reactive Balance System uses a
computer-controlled, multidirectional platform to
challenge balance and reactions.
Impaired balance and postural control commonly affect the safety and mobility of patients with stroke, resulting in an increased risk for falls. A wide variety of balance technologies is available to address the complex nature of balance deficits.
A technology to consider is the Proprio Reactive Balance System by Perry Dynamics, based in Decatur, Ill. According to www.perrydynamics.com, “The Proprio Reactive Balance System uses a computer controlled, multi-directional platform to challenge balance and reactions. The platform generates perturbations to provide variable surface movement requiring the patient to react to their environment.”
Another balance technology is the 3D Balance Control Trainer by Access Health, Melbourne, Australia. According to a study in 2012 by Lee et al, this balance control system is composed of self-weight shifting exercises and video games that use visual feedback during task-specific lower limb exercises and video games that demonstrate weight shift, not only in the horizontal plane, but also the vertical plane.3
ZeroG by Aretech (referenced earlier) can also be used as a gait training device. The harness system allows the patient to be safe while challenging their balance system. It also frees the clinician’s hands to provide appropriate facilitation and eliminates the need for additional assistance by a rehabilitation technician. Recent research states that virtual reality and gaming can motivate patients to improve their balance. Specific examples of this include the Nintendo Wii Balance Board and virtual reality balance training combined with gaming.
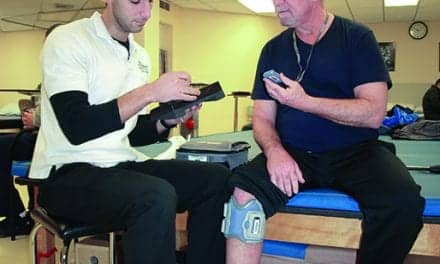
Functional Electrical Stimulation Devices
Approximately 50% to 60% of stroke survivors demonstrate some degree of motor impairment resulting in decreased independence with activities of daily living and increased risk for falls.4 Functional electrical stimulation (FES) devices offer an alternative treatment approach to addressing foot drop, a common potential cause of falls. There are two different types of custom fit, neuroprosthetic functional electrical stimulation devices, including the Bioness L300 (for foot drop) and L300 Plus (for thigh weakness) available through Bioness Inc, Valencia, Calif, and the WalkAide by Austin, Texas-based Innovative Neurotronics. Both the Bioness L300 and the WalkAide are wireless technologies that use a foot sensor and surface electrodes to stimulate the peroneal nerve to facilitate ankle dorsiflexion during swing phase of the gait cycle.
Another FES device, the RT300 FES Cycle by Restorative Therapies, Baltimore, is engineered to provide electrical stimulation of up to 16 muscle groups in the patient’s legs and trunk in a cyclical pattern. A computer monitor tracks data and allows clinicians to tailor individualized training programs for each patient.
Bracing
A more traditional treatment option to address foot drop, compared to electrical stimulation, is the use of an ankle foot orthosis (AFO). Custom plastic solid or hinged ankle foot orthoses are one type of bracing option that will control foot drop and medial and lateral instability of the ankle, while also preventing genu recurvatum. Carbon fiber bracing is a more advanced treatment option that is able to absorb and store energy and is lightweight, but not custom fit. There are several models, including Austin, Texas-based Ottobock’s WalkOn, the Össur AFO Light by Össur, Foothill Ranch, Calif, and the Blue Rocker, available through Allard USA, headquartered in Rockaway, NJ. These braces are appropriate for patients with foot drop and minimal knee control impairments in the mid-stance phase of the gait cycle.
Pressure Mapping Systems
Sparta, NJ-based CIR Systems’ GAITRite temporospatial gait analysis walkway features a portable mat with sensors embedded that record temporal (eg, speed) and spatial (eg, step length, stride length) gait characteristics as the patient walks along the length of the mat. Data is recorded for walking over a level surface only and does not require sensors to be applied to the patient. This system is appropriate for use with patients that have neurological disorders. Additional pressure mapping systems on the market include the Zeno Walkway, from ProtoKinetics, Havertown, Pa, which provides users a 16-level pressure-sensing pad and circuitry, as well as walkway pressure mapping systems from South Boston-based Tekscan.
Conclusion
There are many technology-based options designed to address gait and balance disorders among patients affected by stroke. The common goal of all these technologies is to assist individuals in achieving their highest level of function during their activities of daily living and mobility. Cost containment, staffing needs, and affordability of equipment are all factors to consider when deciding on a device that is most appropriate for a particular setting. PTP
Amy Goldman, PT, DPT, is stroke program manager and physical therapist at Madonna Rehabilitation Hospital, Lincoln, Neb, where she has more than 13 years of experience in neurological rehabilitation, primarily stroke rehabilitation in the Neuro-Developmental Treatment (NDT) Approach for adults with hemiplegia. She has also served as co-investigator on several stroke clinical research trials at the hospital’s Institute for Rehabilitation Science and Engineering.
Cali Carlson, PT, DPT, is an inpatient physical therapist at Madonna Rehabilitation Hospital, where she has more than 5 years of experience in neurological rehabilitation, primarily stroke rehabilitation. She also teaches a lecture on body weight-supported treadmill training at University of Nebraska Medical Center.
For more information, contact [email protected].
References:
1. Go AS et al. Heart Disease and Stroke Statistics – 2013 Update: A report from the American Heart Association. Circulation. 2012; 125: e2-e220.
2. Burnfield JM, Shu Y, Buster T, Taylor A. Similarity of joint kinematics and muscle demands between elliptical training and walking; implications for practice. Phys Ther. 2010;90:1-17.
3. Lee SH, Byun SD, Kim CH, et al. Feasibility and effects of newly developed balance control trainer for mobility and balance in chronic stroke patients: a randomized controlled trial. Ann Rehabil Med. 2012;36(4):521-529.
4. Calautti C, Baron JC. Functional neuroimaging studies of motor recovery after stroke in adults: a review. Stroke. 2003;34:1553-1566.
5. Sullivan K, Klassen T, Mulroy S. Combined task-specific training and strengthening effects on locomotor recovery post-stroke: a case study. J Neurol Phys Ther. 2006;30(3):130-141.
6. Outermans JC, Van Peppen RP, Wittink H, Takken T, Kwakkel G. Effects of a high-intensity task-oriented training on gait performance early after stroke: a pilot study. Clin Rehabil. 2010;24(11):979-987.