Cleveland Clinic was awarded $5.5 million from the National Institutes of Health to develop a stem cell treatment for complex regional pain syndrome, a disease that causes debilitating chronic pain.
The research shows long-term potential for providing patients suffering from chronic pain an alternative to addictive treatments like opioids.
This is the first federally funded project to develop a therapy using human mesenchymal stem cells (hMSC) in pain management and the largest grant to investigate complex regional pain syndrome. The disease often follows a localized injury, typically an arm or leg, and leads to debilitating chronic pain, swelling, color change and unbearable sensitivity to touch. The symptoms can be so severe that getting dressed or laying down to sleep can be difficult and painful.
Experts believe complex regional pain syndrome results from dysregulating neuroimmune pathways that regulate pain. Painkillers, antidepressants, nerve blocks and lifestyle changes typically have limited effects in managing symptoms, but delivering hMSC could potentially regulate the disease processes causing the chronic pain.
“Unlike pain caused through tissue damage, which is often short-term, neuropathic pain is extremely difficult to treat,” said Jianguo Cheng, MD, PhD, medical director of Cleveland Clinic’s Consortium for Pain (C3P), the principal investigator on the grant. “This is an unprecedented opportunity to tackle this major problem using a novel mechanism guided by cellular interactions and addressing the condition on a cellular and molecular level.”
Mesenchymal stem cells are adult stem cells found in various tissues, including bone marrow and fat. These cells have been shown to have powerful immune-modulatory functions when transplanted.
Previous research on complex regional pain syndrome identified an autoimmune component to the disease, which hMSC have the potential to regulate through cell-to-cell communication and secreting substances that can modify immune system functions. Dr. Cheng’s team plans to manufacture clinical-grade stem cells and design an approach for delivering them to patients using preclinical models. Once that strategy is developed, the research would move to clinical trials.
This project includes co-investigators from Cleveland Clinic Departments of Outcomes Research and Pain Management, Case Western Reserve University and Mayo Clinic.
If hMSC works for complex regional pain syndrome, the delivery could open up stem cell treatment options for other patients suffering from chronic pain, Dr. Cheng says. More than 50 million American adults are afflicted with chronic pain, which can lead to problems like insomnia, mood disorders and opioid abuse.
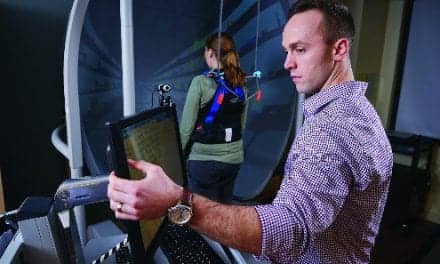
Co-investigators on the project include multiple members of Cleveland Clinic’s Consortium for Pain (C3P), designed to connect clinicians and researchers with expertise that can support pain management research, including neuro-immunology, genomics and anesthesiology. Collaborative pain research can bring together essential perspectives for understanding the challenges of treating chronic pain on a deeper scientific level, said Carl Saab, PhD, Biomedical Engineering, the consortium’s founder and scientific director.
“Unmanaged pain necessitates escalating drug treatment to opioid use,” says Dr. Saab, who is a consultant for the complex regional pain syndrome project and the director of Cleveland Clinic’s Pain Science Technology and Research (STAR) Lab. “Because we don’t have good pain management therapies – we haven’t had any breakthrough drug on the market in decades – research becomes pivotal.”
[Source(s): Cleveland Clinic, EurekAlert]