The International Association for the Study of Pain (IASP) has revised the definition of pain for the first time since 1979, the result of a years-long process that the association hopes will lead to new ways of assessing pain.
The revised definition, along with the associated commentary by President Lars Arendt-Nielsen and Immediate Past President, Judith Turner, was published recently in the association’s official journal, PAIN.
“IASP and the Task Force that wrote the revised definition and notes did so to better convey the nuances and the complexity of pain and hoped that it would lead to improved assessment and management of those with pain. Pain is not merely a sensation, or limited to signals that travel through the nervous system as a result of tissue damage,” he said. “With a better understanding of an individual’s pain experience, we may be able to, through an interdisciplinary approach, add a variety of therapies to personalize their treatment of pain.”
— Srinivasa N. Raja, MD, Chair of the IASP Task Force and Director of Pain Research, Professor of Anesthesiology & Critical Care Medicine, Professor of Neurology, Johns Hopkins University School of Medicine
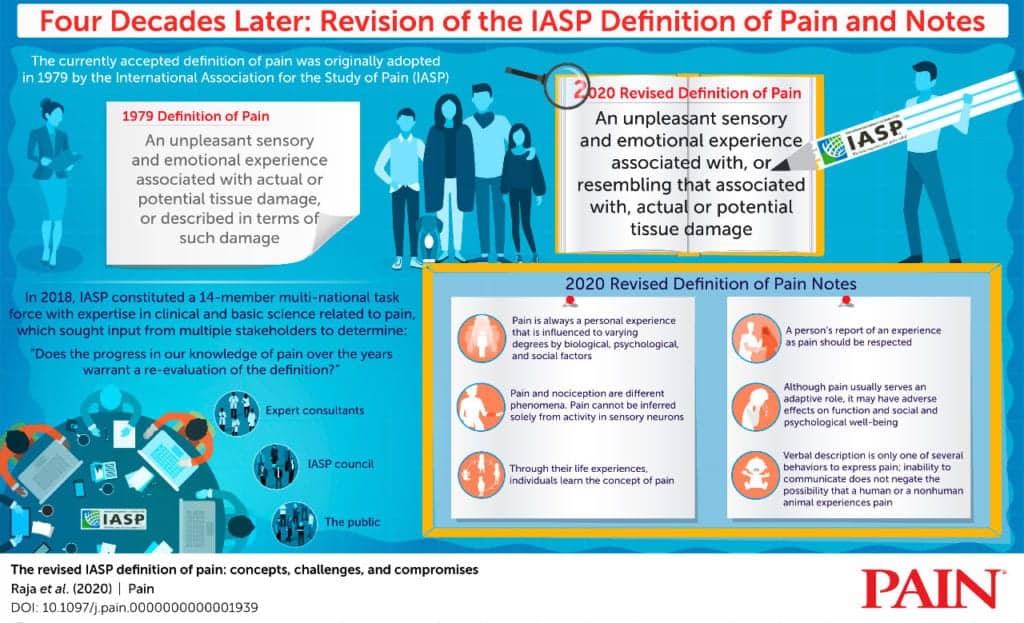
The revised definition is “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage,” and is expanded upon by the addition of six key Notes and the etymology of the word pain for further valuable context, IASP notes in a media release:
- Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
- Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.
- Through their life experiences, individuals learn the concept of pain.
- A person’s report of an experience as pain should be respected.
- Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being.
- Verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain.
Etymology: Middle English, from Anglo-French peine (pain, suffering), from Latin poena (penalty, punishment), in turn from Greek poinē (payment, penalty, recompense).
A central change in the revised definition, compared to the 1979 version, is replacing terminology that relied upon a person’s ability to describe the experience to qualify as pain.
“The old definition read: ‘An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.’ This wording was interpreted as excluding infants, elderly people, and others – even animals — who could not verbally articulate their pain.”
— Dr Jeffrey Mogil, Director of the Alan Edwards Center for Research on Pain, McGill University and member of the Task Force
The six points that comprise the Notes to the revised definition are a key modification.
“They emphasize the three intertwined dimensions of the experience of pain- biological, psychological, and social, and the personal learned nature of that experience.”
— Dr. Milton Cohen, St. Vincent’s Clinical School, UNSW Medicine, Sydney, and member of the Task Force
The notes highlight that pain may have adverse effects on function and social and psychological well-being. One result of that distinction may be that the standard way a person describes pain – using a scale of 0-10 – may be updated to include whether a person’s pain interferes with work, maintaining healthy relationships, daily living, and other psychological and social measures, Dr Bonnie Stevens, Lawrence S Bloomberg Faculty of Nursing, Faculties of Medicine and Dentistry, University of Toronto, and member of the Task Force, explains, the release continues.
The 1979 IASP definition of pain has become accepted globally by health care professionals and researchers in the pain field, and has been adopted by several professional, governmental, and nongovernmental organizations, including the World Health Organization, according to the article in PAIN.
Although subsequent revisions and updates have been made to the list of associated pain terms over the years, the IASP definition of pain itself has remained unchanged until now. In recent years, leaders in the field have voiced that advances in the understanding of pain in its broadest sense warrant a formal re-evaluation of the definition.
“We included the etymology of the word pain because it frames our entire reference point; this English word stems from a Greek root meaning penalty or punishment. Other words in daily use by the ancient Greeks emphasized pain’s location or the distress it may cause. We would do well to return to thinking about pain as having multiple dimensions, so that we can assess and treat it more holistically.”
— Task Force Member Dr Dan Carr, Program in Public Health and Community Medicine, Department of Anesthesiology and Perioperative Medicine, Tufts University School of Medicine, Boston
“The revised definition was a true collaborative effort, written by a multi-national, multidisciplinary task force that received input from numerous stakeholders, including persons in pain and their caregivers.”
— Srinivasa N. Raja, MD
Members of the task force:
- Chair: Srinivasa Raja, MD, Department of Anesthesiology and Critical Care Medicine, Johns Hopkins University, School of Medicine, Baltimore, MD, United States
- Dan Carr, MD, Program in Public Health and Community Medicine, Department of Anesthesiology and Perioperative Medicine, Tufts University School of Medicine, Boston, MA, United States
- Milton Cohen, MD, St Vincent’s Clinical School, UNSW Medicine, Sydney, New South Wales, Australia
- Nanna Finnerup, MD, Department of Clinical Medicine, Danish Pain Research Center, Aarhus University, Aarhus, Denmark, Department of Neurology, Aarhus University Hospital, Aarhus, Denmark
- Herta Flor, PhD, Institute of Cognitive and Clinical Psychology, Central Institute of Mental Health, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany
- Stephen Gibson, PhD, Caulfield Pain Management and Research Centre, University of Melbourne, Melbourne, Australia
- Francis Keefe, PhD, Duke Pain Prevention and Treatment Research Program, Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine, Durham, NC, United States
- Jeffrey Mogil, PhD, Departments of Psychology and Anesthesia, McGill University, Montreal, QC, Canada
- Matthias Ringkamp, MD, PhD, Department of Neurosurgery, Johns Hopkins University, School of Medicine, Baltimore, MD, United States
- Kathleen Sluka, PT, PhD, Department of Physical Therapy and Rehabilitation Science, University of Iowa, Iowa City, IA, United States
- Xue Jun Song, MD, PhD, SUSTech Center for Pain Medicine, Southern University of Science and Technology School of Medicine, Shenzhen, Guangdong, China
- Bonnie Stevens, RN, PhD, Lawrence S Bloomberg Faculty of Nursing, Faculties of Medicine and Dentistry, University of Toronto, Toronto, ON, Canada
- Mark D. Sullivan, MD, PhD, Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA, United States
- Takahiro Ushida, MD, PhD, Multidisciplinary Pain Center, Aichi Medical University, Nagakute, Japan
[Source(s): International Association for the Study of Pain, PR Newswire]
Related Content:
Treating Persistent Pain
Study Touts ‘Supportive Touch’ as a Pain Reducer in Women
Tapping Into Pain: A Product Approach