By Kanika Govil, MPT, C/NDT, C/IASTM
Stroke is among the most common causes of adult-onset disability. The worldwide prevalence of stroke was estimated to be 33 million in 2010. Research shows that 70% to 85% of first strokes are accompanied by hemiplegia. Also, 6 months after stroke, only 60% of people with hemiparesis who need inpatient rehabilitation have achieved functional independence in simpler activities of daily living.1 Of the 730,000 individuals who survive stroke each year, 73% will have residual deficits in motor control and subsequent limitations in mobility, making stroke the leading cause of disability in the United States.2
Regaining locomotor ability is a primary goal in stroke rehabilitation. Walking ability and ambulatory independence determine the level of disability and likelihood of institutionalization in patients with hemiplegia.3 Early intervention with physical therapy to restore walking after stroke is recommended to improve motor function and decrease disability. But, evidence suggests that even in later stages after stroke, motor performance can improve. Hence, gait training is a main component of physiotherapy within stroke rehabilitation because it is an important criterion for discharge and requirements for functioning at home. A paradigm shift has recently occurred in walking rehabilitation post-stroke to focus more on the nervous system’s ability to recover a normalized movement pattern instead of only teaching methods of compensation for impaired mobility, motor control, and balance.2
Approaches for Walking
One of the more common complaints from patients who are living at home 6 months after stroke is that they cannot yet walk safely and efficiently in the community. The likelihood of recovering the ability to walk 150 feet without physical assistance depends, in part, on the type of stroke-related impairments.
The major requirements for successful walking include:
1) Support of body mass by the LEs
2) Production of locomotor rhythm
3) Dynamic postural control of the moving body
4) Propulsion of the body in the intended direction
5) Adaptability of the locomotor response to changing environmental and tasks demands
These requirements should be performed in an energy-efficient manner to minimize stress on the individual. Clinical researchers have used these findings to develop physical therapy interventions designed to improve locomotor ability in a variety of patient populations. Although the specific interventions strategies vary, they share common principles. The locomotor training principles that guide selection of interventions are:
1) Task-oriented to the specific task of walking
2) Goal-directed and meaningful to the patients
3) Shaped and progressed to maximally challenge the patient’s capabilities
4) Performed multiple times (high number of repetitions)
The application of these principles to the specific locomotor training interventions varies depending on a variety of factors that include patient health condition, prognosis, patient goals, body structure/functional impairments, and weight-bearing status.
[sidebar float=”right” width=”250″]Product Resources
The following companies provide technologies that can be useful in the treatment of stroke and neurological conditions:
Allard USA Inc
www.allardusa.com
Biodex
www.biodex.com
GAITRite/CIR Systems Inc
www.gaitrite.com
Gorbel Rehabilitation
www.safegait.com
Hocoma
www.hocoma.com
Mobility Research
www.litegait.com
ProtoKinetics
www.protokinetics.com
Vista Medical
www.boditrak.com[/sidebar]
Interventions to Improve Gait and Locomotion in Stroke
Task-specific overground locomotor training
Task-specific overground locomotor training focuses on practicing in a variety of activities and improving the quality of walking and walking endurance. Appropriate stretching and strengthening exercises for the LE muscles are important preparatory interventions. Parallel bars and ambulation aids (eg, walkers, hemi walkers, quad canes) can assist in early gait stability and safety. There is increased loading on UEs and stronger LE. The patient should practice functional tasks that include the following:
1) Walking forward: Focus is on moving out of synergy by combining hip and knee extension with hip abduction
2) Walking backward: Focus is moving out of synergy by combining hip extensors with knee flexors
3) Side stepping: Focus is moving out of synergy by combining hip abductors with hip and knee extensors
4) Crossed stepping: The PNF activity of braiding combines side stepping and cross stepping
5) Step-up and step-down activities
6) Stair climbing
7) Walking in a simulated environment: Through doorways, over and around obstacles
8) Walking in a community environment: Walking on ramps, curbs, uneven terrain
9) Dual task activities: Walking while holding a ball, bouncing a ball, carrying a tray
10) Balance activities: Tandem walking, walking on / off the foam
As control develops, patients can be encouraged to improve rhythm and speed of walking. Even steps can be facilitated by the use of real-time, rhythmic auditory cues. Progression is to longer steps and to increase the overall distance with faster speeds.
Locomotor training using a dynamic body weight support ceiling-mounted trolley system
Gait performance is an indicator of mobility impairment and disability after stroke. It has already been proven in many research efforts that gait speed is responsive to short-term rehabilitation. An improvement in gait speed of 0.16 m/s can reduce the level of assistance in patients with subacute stroke and was recommended to be the minimum clinically significant difference. Stroke patients often have gait impairments such as decreased gait speed and asymmetrical gait cycle as a result of cortical reorganization. Repetitive mass motor practice task practice had been shown to facilitate neuroplasticity and brain reorganization in stroke patients, resulting in enhanced motor recovery after stroke.
Body weight supported training (BWST) is a task-oriented technique for gait restoration. BWST has the advantage over conventional therapy as it offers higher intensity, more repetitive and task-oriented practice over the same period of time when compared to conventional therapy. Several studies have shown that BWST was more effective in gait speed improvement than regular physiotherapy. It has also been proven that BWST induces changes in cortical excitability, which lead to improved balance and gait performance with chronic stroke.
Many studies about locomotor training have been done to promote normal motor patterns that include BWS treadmill training, overground gait training, and partial body weight support during overground walking. Most of these studies have been done for a longer period of time (6 weeks or more) and have not assessed the association of training with improvement in balance and gait parameters other than just walking speed. There is considerable evidence of gait training being imparted through conventional physical therapy techniques and using the latest technology instrumentation. But, there is still little evidence as to how dynamic body weight support training using a ceiling-mounted robotic trolley system affects the gait parameters and balance confidence in patients with stroke.
Over-ground gait and safety system: a new addition
While body weight support technologies are not new to the rehabilitation community, the ongoing research and development among the manufacturers of these technologies brings a consistent stream of improvement to this product category. Dynamic body weight support devices are available to the physical therapy market from several sources, including Hocoma, Norwell, Mass, which manufactures the Andago, a mobile frame that allows the user to perform self-directed walking over ground while providing fall protection.
Another system in this category is the Vector Over Ground Gait and Safety system from Bioness Inc, Valencia, Calif, one of which was recently put into operation at Encompass Health Rehabilitation Hospital, Dallas. This device is designed to accommodate patients who weigh up to 500 pounds and provide active body control fall protection. The Vector is ceiling mounted and can accommodate up to three robotic trolleys on a single track and can be operated remotely or from a computer. Following are the key clinical benefits the Vector provides to this facility:
1) Empowers therapists to develop more effective and challenging treatment regimes
2) Promotes earlier task-specific mobility by providing a safe environment to practice pre-gait activities, over-ground gait rehabilitation and ADLs
3) Leverages dynamic body weight support to promote early intervention and faster gait rehabilitation
Dynamic body weight support (DBWS) provides consistent unloading to a patient during center of mass elevations and depressions. The use of DBWS instills confidence and enables the patient to replicate natural kinematic movements without the fear of falling.
Case Studies
Three case studies were performed with stroke patients at Encompass Health Rehabilitation Hospital, Dallas, to investigate the effect of 2 weeks of body weight support overground training using a ceiling-mounted, robotic trolley system on gait parameters and balance confidence in subacute and chronic stroke patients.
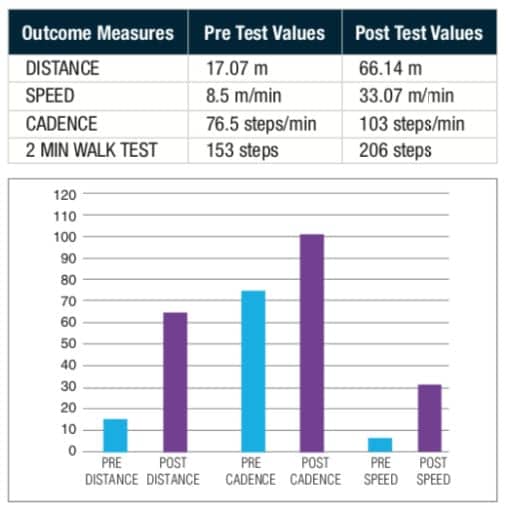
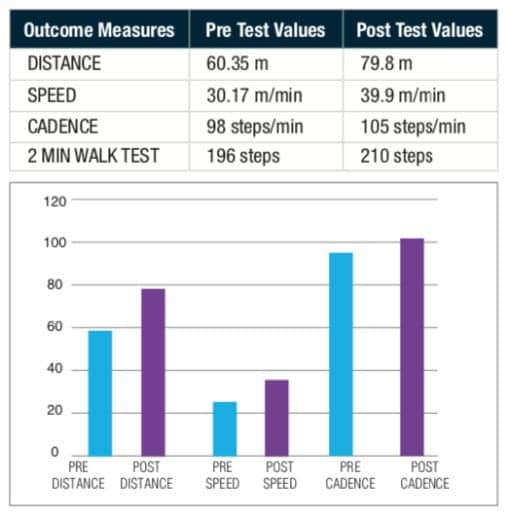
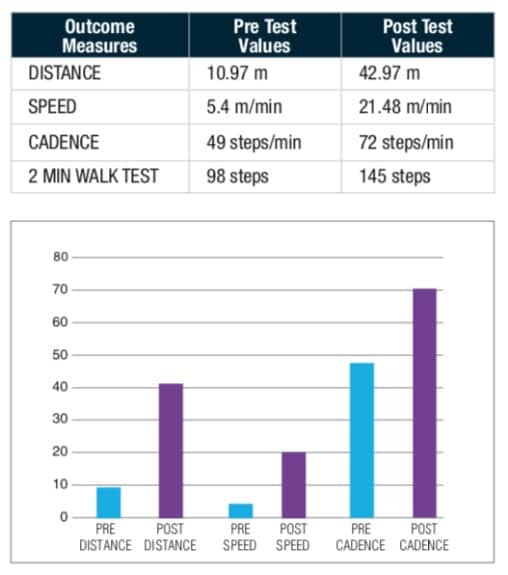
Intervention: Pre-test step length, walking velocity and cadence testing was done using a 2-minute walk test. Balance confidence scores were taken using the ABC scale. Three patients who met the inclusion criteria were given gait training using the Vector Gait and Safety System for 5 days per week/30 min per day for 2 weeks in conjunction with regular conventional physical therapy. After 2 weeks, post-test scores were taken. Comparison of pre-test and post-test scores was done to quantify the gains in distance, speed, and cadence.
Case Study 1
Patient is a 68-year-old male admitted to acute care after falling at home. Patient reports he laid on the floor for 4 days and presents with a subacute right frontal lobe ischemic infarct found on CT head. MRI Brain: Acute right frontal lobe infarction with extension to right insular cortex. PMH: DM2 and asthma.
Case Study 2
Patient is a 61-year-old male who presents with impaired functional mobility secondary to AMS and remote basal ganglia infarcts and chronic microvascular ischemic changes. Patient presents with complaints left-sided facial drop and right leg weakness, right-sided paresthesia, slurred speech, and intermittent numbness. MRI Brain reveals Lacunar stroke. PMH: Chronic gout, HTN, HLD.
Case Study 3
Patient is a 73-year-old male admitted after acute onset of chronic traumatic subdural hematoma status post right frontal/parietal burr holes with acute infarcts in multiple vascular territories and multiple falls.
MRI Brain reveals recent ischemic changes with right temporal lobe and overlying frontal operculum. PMH: Diabetes, HTN, Hypothyroid.
Results and Clinical Implications
Results suggested that 2 weeks of gait training using dynamic body weight-supported overground training using a ceiling-mounted trolley system can improve the gait parameters in patients with subacute and chronic stroke.
Since the average length of stay in any inpatient rehabilitation facility is 2 to 3 weeks, these case studies investigated the effect of 2 weeks of dynamic body weight support gait training on both temporal and spatial gait parameters. This study also helped determine the effect of intensive gait training on the discharge outcomes of the patients, thereby promoting more community discharges with fewer incidence of falls and readmission to the facility. PTP
Kanika Govil, MPT, C/NDT, C/IASTM, is the physical therapy team lead at Encompass Health Rehabilitation Hospital, Dallas, Texas. Her experience includes treating spinal cord injury and neurodevelopmental treatment in stroke. For more information, contact [email protected].
References
1. Wonsetler EC, Bowden MG. A systematic review of mechanisms of gait speed change post- stroke. Part 2: Exercise capacity, muscle activation, kinetic and kinematics. Top Stroke Rehabil. 2017;24(5):394-403.
2. Li-Juan Jie, Melanie Kleynen. The effects of implicit and explicit motor learning in gait rehabilitation of people after stroke: Protocol for a randomized control trial. JMIR Research Protoc. 2018;7(5):e142.
3. Bruce H Dobkin. Strategies for stroke rehabilitation. Lancet Neurol. 2004;3(9):528-536.
4. Mao YR, Lo WL, Lin Q, et al. The effect of body weight support treadmill training on gait recovery, proximal lower limb motor pattern, and balance in patients with Subacute stroke. Biomed Res Int. 2015;2015:175719.
5. O’Sullivan SB, Schmitz TJ, Fulk GD. Physical Rehabilitation. 6th Ed.
The Crystal Ball of Gait
Advanced sensing technologies help therapists zero in on the early signs of disease-related impairmentBy Frank Long, MS, Editorial Director, Physical Therapy Products
You can tell a lot about people by the shoes they wear. That advice has propped up judgements about a person’s wealth, vocation, and athletic ability for a very long time—perhaps since shoes were invented. But while your footwear can rat out who among your family members tracked mud across the floor, they fall short in their ability to predict health. Gait is another matter, however, and the nuances of a person’s walk can speak volumes about an individual’s physical condition.
What Gait Says About Neurodegenerative Disease
Parkinson’s disease is no stranger to physical therapy. According to recent statistics published by the National Institutes of Health, approximately 50,000 people are diagnosed with the neurodegenerative disorder each year, and an associated late motor complication is freezing of gait (FOG). Reports in the medical literature show that up to 80% of Parkinson’s disease patients will be affected by this common axial symptom during the course of the disease. Add to that how poor quality of life and disease severity correlate with FOG, and it becomes clear that detecting FOG early could be useful in designing long-term strategies.
So, how to predict FOG? One approach is detailed in a 2017 report by University of Arkansas-based researchers Tuhin Virmani, MD, PhD, and Jesal Shah, MD, who evaluated whether steady-state gait parameters in Parkinson’s disease could be used as a predictive biomarker for FOG. A critical part of their testing include data capture by the Zeno Walkway, manufactured by ProtoKinetics, Havertown, Pa. As part of their study, Vermani and Shah enrolled 70 age-matched subjects who walked at a normal pace for eight rounds on the Zeno Walkway’s pressure-sensitive mat.
Virmani and Shah found that the Parkinson’s disease patients they tested who were affected by FOG had decreased stride length and stride velocity. The researchers likewise reported those study subjects had “increased variability in stride length and stride velocity, but not total double support or stance percent.” Virmani and Shah concluded that the differential regulation suggested objective gait assessment could offer an avenue by which clinicians might predict FOG among individuals affected by Parkinson’s disease.
Early Detection for Multiple Sclerosis
The importance of early disease detection cannot be overstated. It is desirable across the board for diagnosing chronic illnesses such as multiple sclerosis, for which early detection provides significant advantages in managing long-term disability. A multiple sclerosis diagnosis may be slow in coming since there is no testing available to confirm its presence and symptoms can be non-specific. The disease also can cause early damage in the central nervous system before an affected individual experiences symptoms. Both factors make early identification especially crucial, which underscores the importance of technologies that identify the subtle gait and balance dysfunction that attend multiple sclerosis.
In 2017 Frontiers in Neurology published a study led by Camille J. Shanahan, MSD, University of Melbourne, that performed a head-to-head evaluation of technologies designed to conduct advanced gait and balance assessments among people affected by multiple sclerosis. Among those technologies were instrumented walkway mats such as the GAITRite from CIR Systems, Franklin, NJ, part of a device category the researchers considered to generally provide the most sensitive and accurate gait data.
Shanahan and her team reported that the GAITRite had a high sensitivity for detecting pathology-related changes. The device was able to determine spatiotemporal measures of gait—including walking speed, step and stride lengths; base of support; step, stride, swing, stance, single support, and double support times; and toe in/out angle. The development path for this technology, the authors concluded, would allow them to monitor and predict disability associated with multiple sclerosis in real-world environments.
Headed for a Fall?
Aging increases fall risk, and advanced age is ranked by the Centers for Disease Control and as one of the top intrinsic factors that can precipitate a fall. As individuals approach retirement age and conversations about health and active aging become more common, an aging person’s interest in a fall prevention program may escalate. This is where a PT clinic can provide an important pre-emptive service.
One technology therapists can use to form a data-supported view of fall risk is a floor- or treadmill-based pressure mapping system. BodiTrak, from Vista Medical, Winnipeg, Manitoba, Canada, is a pressure-sensing pad with a relatively small footprint that can measure equilibrium, firmness, and active stability. BodiTrak is engineered to track the center of pressure and calculate total and maximum distance in addition to velocity. The system’s software and pressure-sensing pad generate data therapists can use to identify challenges with balance that may result from stroke or other insults.
Subtle threats forming within muscle, bone, and the central nervous system may evade the human eye but will be much less successful in hiding from advanced sensing technologies. Although the future is never certain, the ability for clinicians and patients to use these technologies to harness objective data that will help their patients manage and minimize fall risks seems to be a sure thing. PTP