How the use of technology for post-stroke patients leads to better assessments, more effective interventions, and efficient care outcomes
By Emily Lyter, PT, DPT
Stroke is a leading cause of disability in the United States and can have wide-ranging effects on an individual’s life and participation in family and social roles. The latest epidemiological evidence suggests one person has a stroke every 40 seconds, and 7 million people in the United States are stroke survivors.1,2
A person who suffers a stroke can face lasting effects on his or her ability to perform daily activities and move around in the home and community. Typically observed impairments include unilateral weakness, impaired muscle tone, altered sensation, and altered motor planning. These impairments can lead to an increased risk of falls and a decreased gait speed, requiring higher energy expenditure.3
Over the last two decades, rehabilitation technology has greatly expanded options for assessment and treatment of individuals who are post-stroke. Good Shepherd Rehabilitation Network (GSRN) in Allentown, Pa, specializes in the rehabilitation of individuals who have had a stroke at each phase of their recovery. GSRN’s comprehensive stroke program integrates specially trained clinicians and the use of technology to improve the quality of assessment, effectiveness of interventions and efficiency of care outcomes.
[sidebar float=”right” width=”250″]Product Resources
The following companies provide technologies that can be useful in the treatment of stroke and neurological conditions:
Allard USA Inc
www.allardusa.com
Clarke Health Care Products
www.clarkehealthcare.com
DIH
www.dih.com
GAITRite – CIR Systems Inc
www.gaitrite.com
Hocoma
www.hocoma.com
M.A.S.S. Rehab
www.massrehabinc.com
Mobility Research
www.litegait.com
ProtoKinetics
www.protokinetics.com
REAL System
www.realsystem.com
Vista Medical
www.boditrak.com
Z Axis Unweighting
www.zaxisunweighting.com[/sidebar]
Better Baselines and Focused Interventions
During initial evaluation, physical therapists assess how an individual stands, transfers, and walks. Depending where in the brain the stroke is located, patients also may report complaints of dizziness. The availability of infrared video goggles enables therapists to more precisely assess ocular movements that relate to a central or vestibular pathology. Accurate assessment and interpretation of these movements enable a targeted treatment of the underlying pathology or referral to additional medical services as needed.
A sensory organization test can provide a detailed characterization of balance responses. Individual scores for visual, vestibular and somatosensory components of the balance system can help therapists select more specific treatment strategies to the person’s identified deficits. Computerized posturography also will reveal deviations in the location of the person’s center of mass that may indicate asymmetric limb loading. Moreover, comparisons to age and height-matched norms helps therapists set goals and justify continued need of skilled services.
Identified impairments in center of mass or balance strategies can inform the types of interventions a physical therapist selects during the course of care. Selecting activities that preferentially challenge the visual, vestibular or somatosensory systems reduces time spent focusing on the system that may be functioning adequately. This can reduce the number of items provided for a home exercise program and result in improved compliance with balance training outside of the therapy setting. Reassessment using the same sensory organization test allows the physical therapist and patient to quantify the extent to which the individualized exercise program impacted the patient’s balance response.
Using Feedback in Therapy
Physical therapists utilize various methods to help a person learn a new walking pattern, transfer technique or other motor pattern. Through various types of feedback, a clinician can educate a person about the portions of movement that should be modified or sustained. Two commonly used and studied types of feedback include internal and external feedback: Evidence suggests learning a new or modified motor pattern is improved through the use of external feedback.4 Integrated virtual reality and external feedback provided by computerized posturography and gait mapping technology can improve the patient’s engagement and help maximize learning during post-stroke rehabilitation.
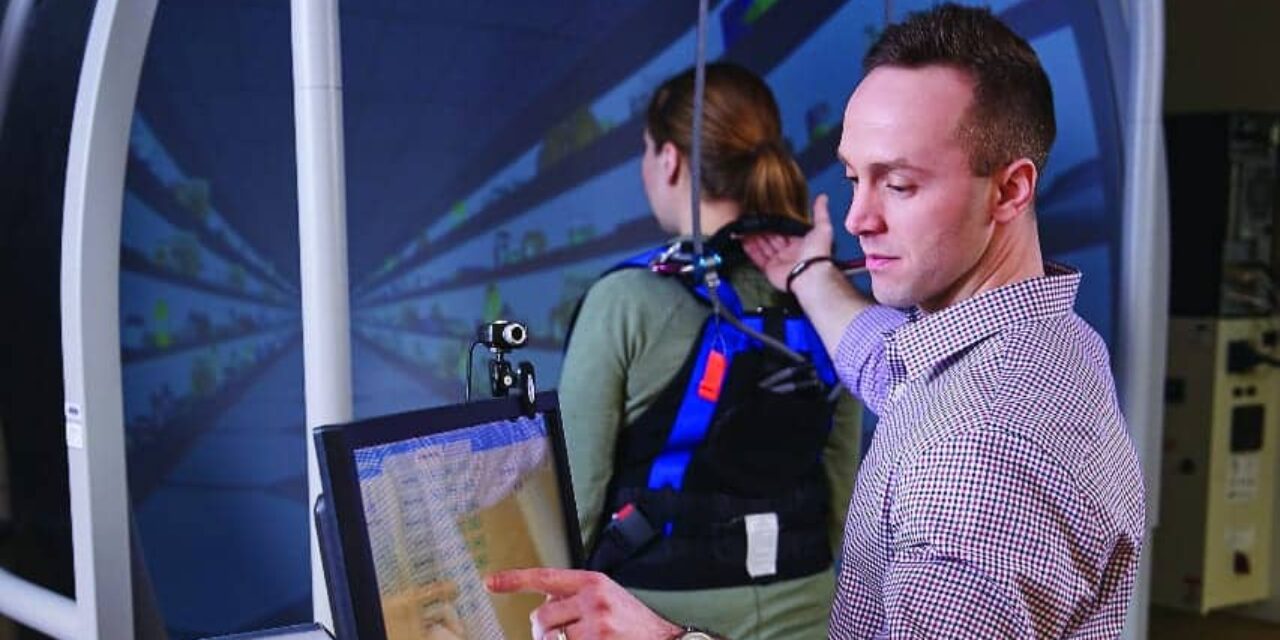
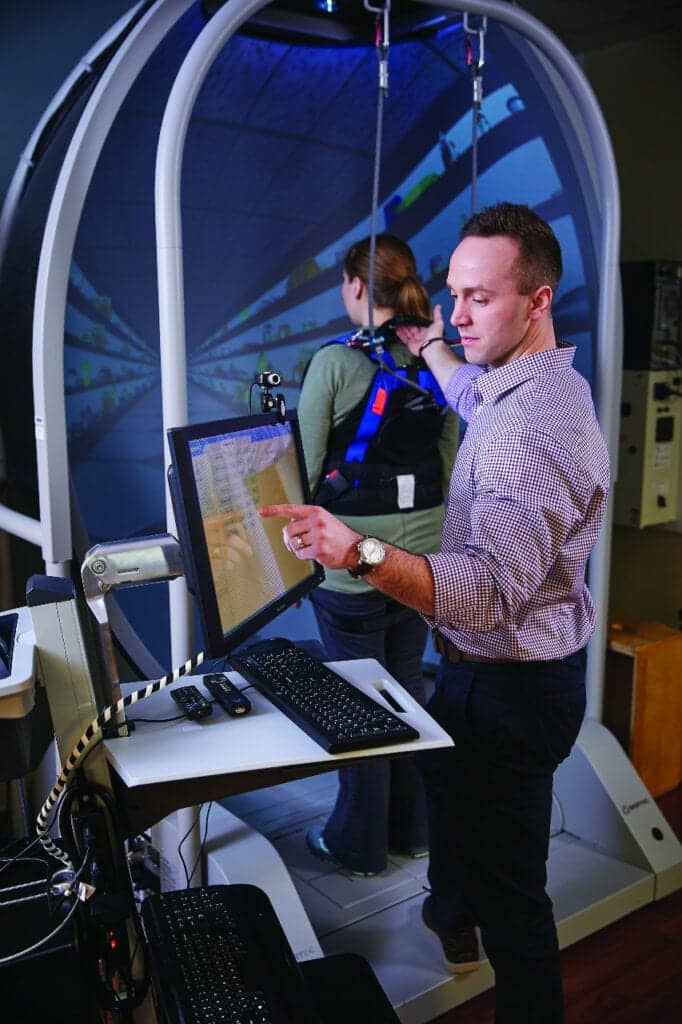
A person recovering from stroke may preferentially stand on the non-hemiparetic limb to increase stability and confidence during upright tasks. To improve symmetrical weight-bearing using internal feedback, a therapist could say, “Put more weight on your right foot.” Using information from computerized posturography, clinicians can provide the same information using external feedback by having the patient move a cursor displayed on a screen. Instead of asking the patient to put more weight on their right foot, the therapist could say, “Move the cursor to the target on the right.” Immersive virtual experiences available through interactive computerized posturography can take this to the next level with the use of a first-person flight simulation by using the transfer of weight from one leg to the other as a means to control a plane flying through targets or navigating through a grocery store or castle. Through subsequent reassessments, therapist and patient can observe changes in weight distribution using graphical and numeric representations along with patient experience and qualitative assessment of mobility tasks. Addressing weight asymmetry while standing in a supportive environment is beneficial for the person to relearn how it feels to stand on that leg and ultimately increases confidence in using the leg. The natural progression is to take the relearned ability to stand on the hemiparetic leg into a functional activity such as walking.4
Gait Analysis
Availability of clinic-friendly gait analysis using a force mat and specialized software can assist in identifying and quantifying abnormal walking patterns. Specific gait deviations occur during different phases of the gait cycle. The ability to know exactly when they occur can be challenging if many deviations coexist in a fast-paced gait, or in a person who may only be able to walk a short distance once. The level of experience a physical therapist has is also a factor in proper assessment of gait quality. The ability to play a video at slow speed and toggle between different phases of gait helps visualize previously undecipherable deviations for both new and experienced clinicians.
Video feedback is particularly helpful for patients to appreciate postural and gait deviations. Differences in shoulder height or lateral movement of the trunk may be easy to visualize in a video if the impairment is significant. For individuals who may be unable to visualize a decrease in weight shift to the right, use of graphical or numerical representation of this difference from the force mat can be more obvious.
Post-walk feedback provided by the physical therapist using quantitative methods to support and visualize the information can then be used by patients to modify their technique. Subsequent walks and external feedback can help patients better understand the sensation of the “better” walking technique, which they can then replicate in and out of therapy.
After a stroke, some patients may require the use of an assistive device or orthosis to provide stability and improve safety when walking. Spatiotemporal parameters and video feedback from quantitative gait assessment can help inform the clinical decision-making regarding the best device and orthotic. Force mat assessment during walking also can be used to inform prescription of prisms to address midline shift abnormalities.

Frequent Reassessment
Bi-weekly or monthly reassessment via objective measurement can provide an unbiased assessment of therapy interventions and keep patient progress at the forefront. Comparison of initial and follow-up performance on the sensory organization test allows patients an objective assessment of their performance and therapists an assessment of the interventions provided.
Visualization of progress in graphical, numerical or video form can be encouraging to patients and reaffirm to them that their efforts are resulting in identified gains. This information can also help motivate improved, continued compliance with home exercise programs. For individuals who are making gains that are less perceptible, integration of force plate data can encourage patients and provide data to justify skilled services to third-party payors.
Recovery from stroke can occur over the span of months or years. During this time, a patient will interact with many clinicians, and having a consistent assessment helps understand changes that occur between episodes of skilled care.
The Impact of Targeted Intervention and Assessments
The ability to utilize technology to supplement qualitative assessment can provide more responsive measures of change during rehabilitation post-stroke. Visualization of patient progress over the course of care provides motivation and encouragement during recovery and can improve overall patient compliance and outcomes. The ability to screen and identify peripheral versus central nystagmus improves clinical care by ensuring the appropriate referrals are made and treatments will be effective. Computerized posturography not only provides an assessment of balance strategies and asymmetrical weight distribution, but also provides an immersive training environment that improves learning by increasing enjoyment and providing external feedback. Quantitative gait analysis with video feedback captures the effects of identified impairments on walking quality. Video and spatiotemporal information can impact patient learning and inform clinical decisions regarding assistive devices and the impact of therapy interventions. Taken together, these tools help physical therapists improve patient outcomes by providing targeted intervention and assessments that inform clinical decisions and justification of services. PTP
Emily Lyter, PT, DPT, is a physical therapist who specializes in treating neurologic disorders. She is the research & telemedicine program manager at Good Shepherd Rehabilitation Network in Allentown, Pa. For more information, contact [email protected].
References
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209.
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics – 2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596.
- Patterson KK, Parafianowicz I, Danells CJ, et al. Gait asymmetry in community-ambulating stroke survivors. Arch Phys Med Rehabil. 2008 Feb;89(2):304-10.
- Wulf G, Chiviacowsky S, Schiller E, Avila L. Frequent external-focus feedback enhances motor learning. Front Psychol. 2010 Nov;1:Article 190